Future of anaesthesia care
Umeå Institute of Design – 2017, 10 weeks
Team with Yijia Tao and Geert Roumen
With this project, we re-imagined how contextually designed communication tools can enhance communication and collaboration within the medical sector, especially for the anaesthesia team.
In collaboration with Getinge.

Communication is key, but today’s system is not designed for the medical context.
Communication in an OR is key for a good teamwork and patient safety. The anaesthesia nurse often needs to call the anaesthesiologist for advise or to receive authorisation for procedures. But the system for contacting someone outside the OR is not designed for the medical context.
What if the tools used for communication would be designed for the context they’re used in?
Multiple small issues in the workflow could lead to delays and misunderstandings.
Today, binders full of the entire hospitals phone numbers, landline phones, and pagers are used as communication tools. These can become misplaced in stressful situations. Patient’s vitals, types of medicines, and amounts
are shared over the phone. Especially patient values are hard to communicate properly with just voice and can easily be misunderstood.

Information delay
Information loss hinders to judge the situation correctly
Not possible to communicate the urgency level
Get advice without losing focus on the patient.
Our solution is a tool that makes the communication process more efficient and supports the way of communication already in place.
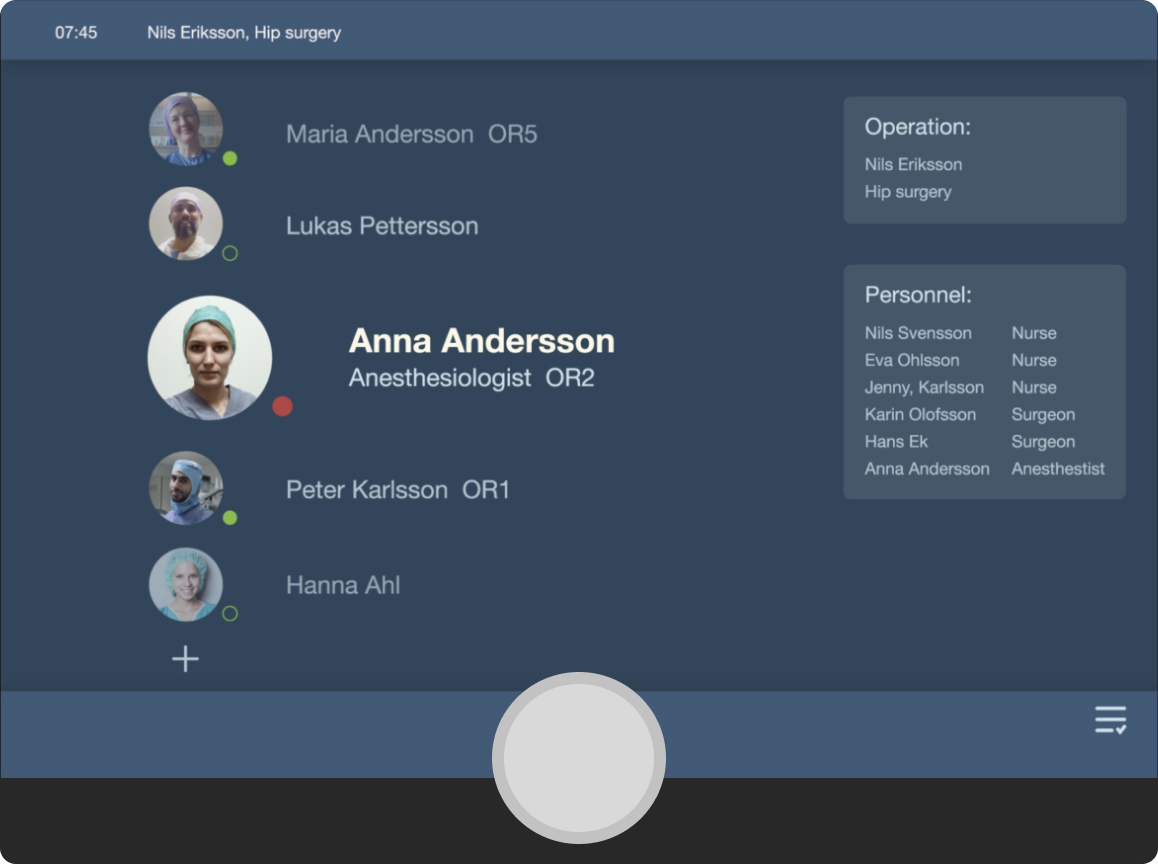
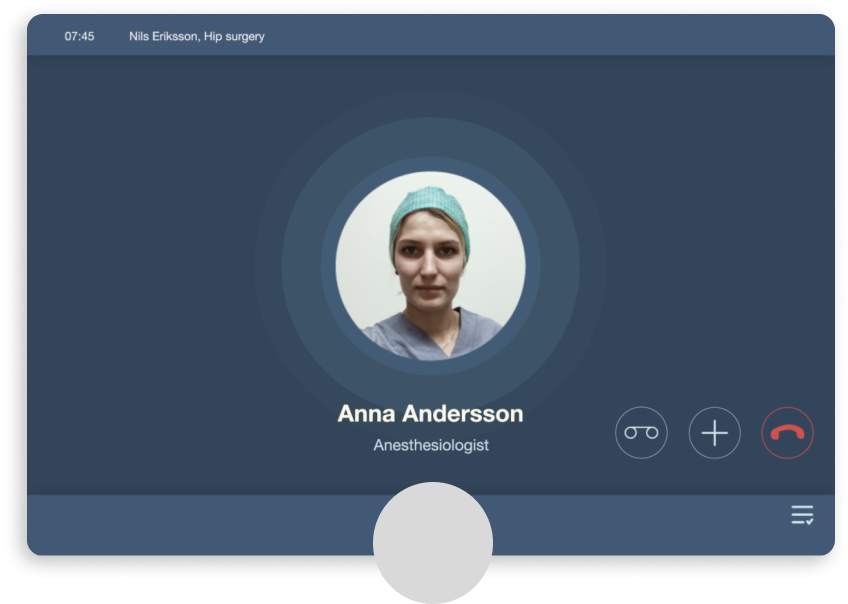
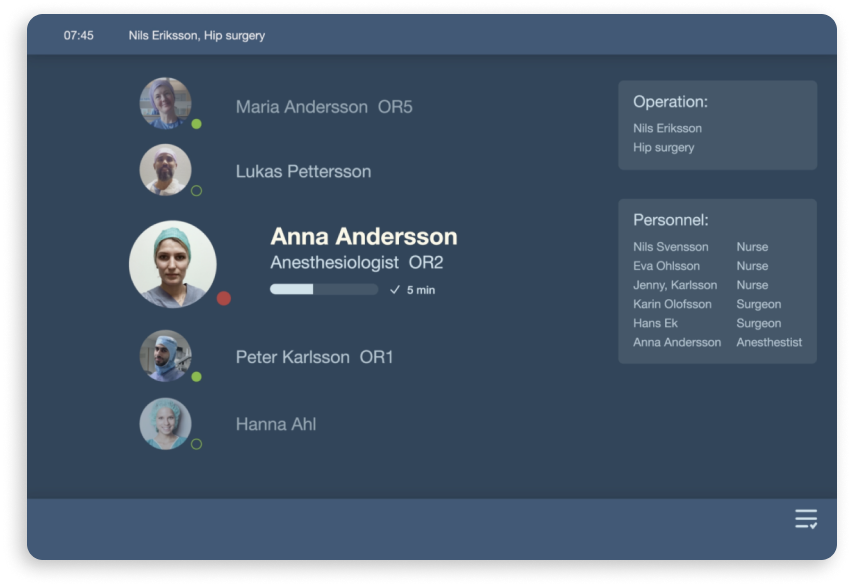
It consists of an operation room device and one personal device for the doctors. Through the OR device, the user can share visual data about the patient while simultaneously attending to the patient. This allows the doctor to quickly give well-informed advice and judge if her presence is required.


Slide, turn, press
Have the doctor on speed dial, inside the OR
The communication device inside the operation room contains information about who to call in case of need or emergency. The speed dial calls adapt to the patient and the type of operation, and the team working.
“I usually write the doctors number on my scrub, to have it easily accessible.” – Anaesthesia nurse
Share urgency level from the start
The user can share the urgency level simultainously as making the call. The receiver of the call then knows how to prioritize. For efficiency, the physical button has three actions built into it, urgency level, contacts, and call. In one simple movement, you can do all of these three actions.
Voice recognition to highlight keywords and suggest actions
The system uses voice recognition during the call to pick up keywords and suggest what to save based on what’s being said, adding an extra layer to the conversation. The users on both ends can then choose to act on it or not.
Instant information sharing
During the call, the team can choose to share the information picked up by the system, such as vitals, medicines, or the amount of blood. It will then be visible for both the sender and receiver on both devices to keep track of the call and be on the same page.
Keep track on what’s next
By moving the bubble to the right, the caller can also save information to act on later. Actions can, for instance, be to order or change the amount of medicine.
Before contact
Speed dial
Make the call
During contact – share information

Shared visual info
Personal notes
After contact – see estimated time of arrival
Timeline


Understanding important interactions and features by involving stakeholders
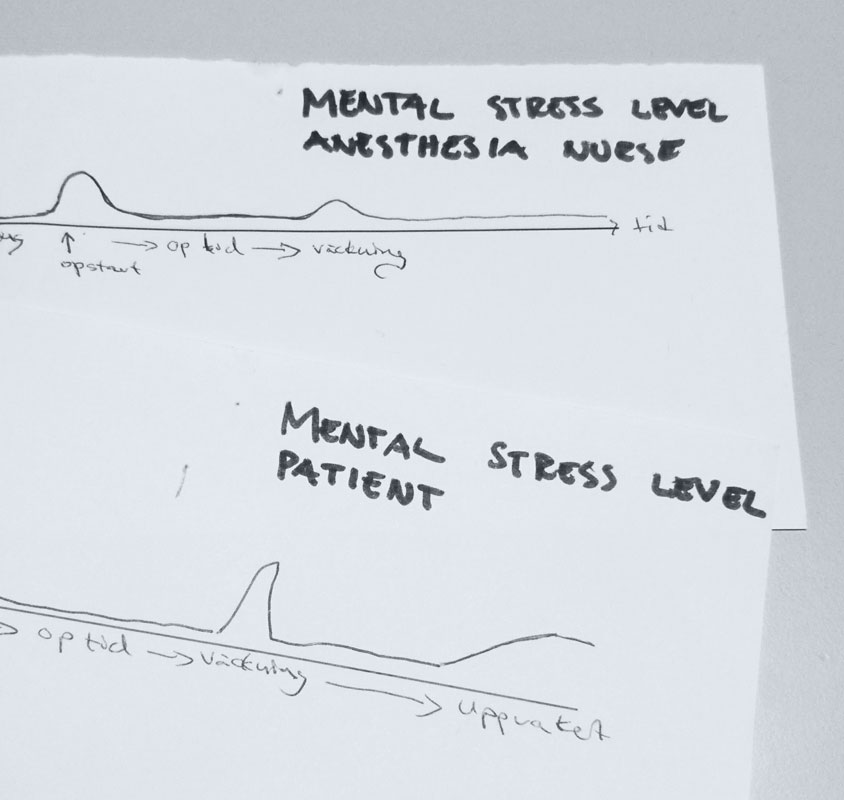
During this project, we got the opportunity to attend several surgeries. It allowed us to understand the flow and critical moments. We continuously involved nurses and doctors as well as our collaboration partner Getinge with whom we shared insights, held workshops, and brainstormed new scenarios.
It resulted in several prototypes that allowed us to explore how they’d fit into users’ daily life. We tested them with the nurses in the OR to make the flow as efficient and usable as possible to handle critical moments. The most crucial features like speed call and urgency level should be the quickest.
15h +
observations and interviews
3
workshops
4
user tests